The vulva refers to the visible or outer parts of the genitalia.
The appearance, shape and size of the vulva can vary from person to person. Most of these variations are normal. It is also normal to have one side of the vulva look slightly different than the other side of the vulva.
The vulva includes the pubic mound, the outer lips, the inner lips and the entrance to the openings of the bladder and vagina. The vagina (or birth canal) is the inner part of the genitalia and is not visible from the outside.
Starting from the top down is the pubic mound or mons pubis. This is a pad of soft fatty tissue above the pubic bone. The skin in this area is covered with pubic hair. Below the mons pubis are the outer lips and inner lips of the vulva.
The outer lips (or skin folds) are large and have pubic hair. These lips are called the labia majora.
The inner lips are smaller and hairless. These lips are called the labia minora. The small lips join together, below the pubic mound to form a hood (or prepuce) above the glans (or tip) of the clitoris. The clitoris is very sensitive. The tip is visible on the outside but a larger portion (the shaft) is not visible.
Between the inner lips of the vulva is the vestibule. The urethra (a tube leading to the bladder) is located in the vestibule above the opening to the vagina. There are a number of glands that open into the vestibule – minor vestibular glands, Skene’s glands and the Bartholin’s glands. These glands produce secretions that make the vestibule moist.
Below the vestibule is the perineum. This skin lies between the opening to the vagina and the opening to the rectum (anus). Many skin conditions that affect the vulva will also affect the skin around the anus or even in between the buttocks.

Once an accurate diagnosis is made, the appropriate medical treatment can be started, however; treating the vulvar skin may not be enough to restore overall health.
Many people with chronic vulvar disorders report that the vulvar condition affects their overall sense of well-being, body image and sexual self-esteem.
A healthy vulva is critical for comfortable daily living activities, such as: sitting, walking, and wearing clothes. If the vulvar skin is unhealthy, it can make urination, menstruation, and/or defecation uncomfortable. A healthy vulva is necessary for pain-free and enjoyable sex.
We understand that individuals who have vulvar symptoms are often too embarrassed to seek help from a health care provider, however; it is often difficult to ignore these conditions. We have outlined below the initial steps to restoring vulvar health.
First Step – Good Skin Care
There are some simple steps that you can do to start improving vulvar symptoms. For some people, vulvar skin care is all that they need. Please see our handout below for recommendations.
Second Step – Find an Expert
Unfortunately, when people do seek help they are often treated over and over again for a suspected vaginal infection. However, vulvar symptoms such as burning, itch or soreness may be due to a skin condition, NOT an infection. In this case, these treatments may in fact make the symptoms worse over time. If you have chronic vulvar symptoms it is important to get an accurate diagnosis. Do not give up. You are not alone.
The second step towards better vulvar health is to see a health care provider with experience in vulvovaginal disorders.
Third Step – Holistic Health
1) Sexual Health: Many who suffer from vulvar disorders have concerns about their sexual health. Some vulvar conditions change the appearance of the vulva and that can make you feel uncomfortable or embarrassed in a sexual setting.
Vulvar diseases can cause significant discomfort when the genitalia are touched. Some people report significant pain with sexual intercourse, reduced sexual frequency and decreased sexual desire. Many avoid sexual activity because of pain, and often choose to be sexually inactive. The avoidance of sex creates interpersonal conflict within relationships, which further compounds the stress of their condition.
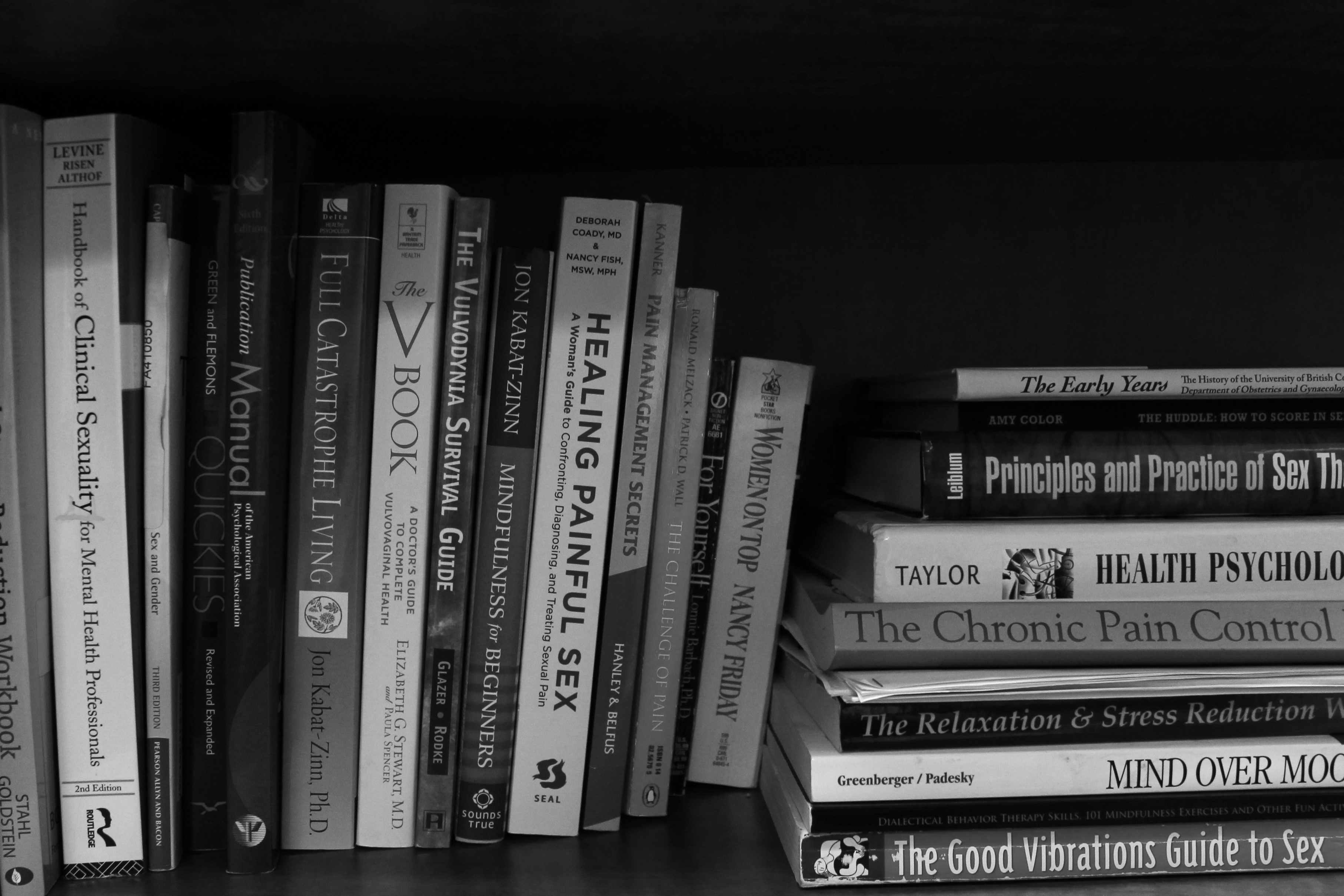
A sexual health expert can help you address these sexual concerns and return to having a fulfilling sexual life.
2) Mental Health: Individuals with vulvar conditions may experience changes to their mental health.
Some may experience embarrassment, fear, anxiety, negative body image, and depression. Some vulvar conditions are associated with a small increased risk of vulvar cancer and thus require long term treatment and follow-up. Some people may have difficulty coping with the need for chronic treatment and surveillance of a condition that affects the genitals.
It has been shown that psychological techniques focused on stress reduction, anxiety control and relaxation have a positive benefit on vulvar pain.
3) Pelvic Floor Physiotherapy: When an individual experiences vulvar discomfort for months and years this can affect their underlying pelvic floor muscles. These muscles can tense up over time. This tension may not disappear when the vulvar condition is treated. Thus, addressing Pelvic Floor Health is an integral part of any treatment plan through the BCCVH.
Thorough physical therapy assessment and treatment addresses all aspects of interdependent pelvic floor function including bladder, bowel, lumbar and pelvic back support, as well as vulvar pain and spasm. It is important to consider all aspects of pelvic floor function as unaddressed pelvic floor dysfunction in one of these areas may limit improvement in another area.
